PolyPharmacy
HI NENC (formerly AHSN NENC) is supporting the delivery of a National Polypharmacy Programme: Getting the Balance Right in partnership with the NENC Integrated Care System (ICS), the national programme to support conversations about medicines between health professionals and the public.
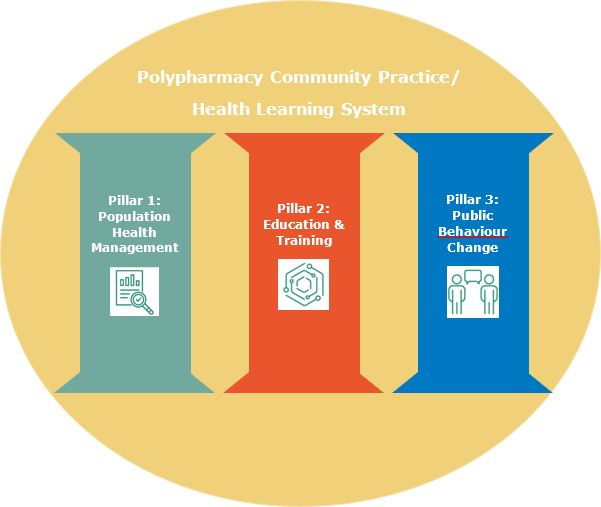
Pillar 1: Population Health Management: Using data (NHS BSA Polypharmacy Comparators) to identify patients for prioritisation for a Structured Medication review.
Pillar 2: Education & Training: Running local Polypharmacy training for the primary care workforce to support stopping unnecessary medicines.
Pillar 3: Public Facing Interventions: Testing patient information developed to support conversations about medicines.
The AHSN NENC has established a Community of Practice in the NENC ICS to:
- Support the delivery of the AHSN National Polypharmacy Programme: Getting the Balance Right
- Foster a culture of engagement, collaboration, learning and innovation to reduce problematic polypharmacy for our population most at risk from harm
- Improve use of resources and reduce duplication
Join the North East and North Cumbria (NENC) Polypharmacy Community of Practice (CoP) on the NHS Futures page.
To drive and accelerate changes in practice, quality improvement projects to address problematic polypharmacy have been shared and collated in a poster repository hosted by Wessex Academic Health Science Network: QI Posters (wessexahsn.org.uk)
If you have any queries regarding this work please contact Emily Whales [email protected]
The projects detailed below were successful in a project call for PolyPharmacy projects. More details about the successful projects can also be found in our Medicines Optimisation brochure.
Download the Medicines Optimisation brochure
PolyPharmacy projects
De-prescribing in Primary Care Getting Started
Despite a wide variety of validated de-prescribing tools being available for use in clinical practice, active de-prescribing in primary care is generally accepted to be low. Feedback from clinicians working in this setting expressed uncertainty about where to start with developing their de-prescribing practice.
The project aimed to work with clinicians across primary and secondary care to co-design tools to support de-prescribing within general practices.
A full report of the project can be downloaded:
Download De-prescribing in Primary Care Report
The full set of ‘Are your medicines working for you’ resources can be found here.
Polypharmacy Education in DDES & N. Durham CCGs
North Durham & DDES Joint M.O. Team, Rachel Berry
1st April 2019 – 31st Jan 2020
The Joint MO Team is proposing to develop and deliver a programme of education to upskill primary care prescribers and practice based pharmacists regarding de-prescribing in key therapeutic areas (cardiovascular, falls, pain, kidneys).
Training slide set:
**All information is up to date as of the end of December 2019, guidance is subject to change. When using after this date, please ensure that the most up to date guidance is used**
1. Introduction to Managing Polypharmacy, and De-prescribing in Cardiovascular Disease
2. De-prescribing in Patients at risk of Acute Kidney Injury
3. De-prescribing in Persistent, Non-Cancer Pain
4. De-prescribing in Patients at risk of Falls
What is the impact of educational interventions on the prescribing of hypnotics at NTW FT?
The aim of the project was to create multi-professional, system-wide educational resources, which can be used as interventions to improve knowledge of sleep and sleep disorder management.
Successful project outcomes include:
- 41% reduction in the number of administrations of hypnotics across the intervention period
- 29% reduction in the number of patients with active hypnotic prescriptions
- Identification of significant areas for improvement, both locally and nationally
- Significant cultural change in prescribing practices, including a more holistic patient assessment and investigation, and wider use of appropriate non-pharmacological interventions.
- Three supportive interventions have been produced: a poster, a video and a handbook (links provided)
This work also feeds into the wider Trust Sleep Well Programme, which aims to implement other holistic interventions such as lighting and estates.
Download the Smarter Sleep Interventions Paper
Reducing antibiotic prescribing through community pharmacy provision
CNE Local Professional Network, Mike Maguire
To test the feasibility of reducing antibiotic prescribing in general practice using the local community pharmacies. Practice receptionists will refer patients who request antibiotics by telephone to community pharmacists for CRP testing, the results of which will inform the consideration of treatment.
A ‘World Cafe’ approach to address the inappropriate prescribing of intravenous antibiotics in futile clinical scenarios
Northumbria Healthcare Trust & Newcastle University, Tanya Miah
1st May 2019 – 30 April 2020
Northumbria Healthcare NHS Trust and the School of Pharmacy at Newcastle University researchers will work together to develop, implement and test ‘Antibiotic Cafes’ with the aim of discussing key clinical issues relating to the prescribing of IVA at the end of life. Healthcare professionals (doctors, nurses, pharmacists and HCPs with an interest in antimicrobial stewardship) and students will be invited to attend the ‘Antibiotic Cafe’.
Antibiotic World Cafe Flash Cards
Antibiotic World Cafe Presentation – Joseph Brayson
Optimising the management of COPD exacerbations in primary care
North West, North Tyneside Primary Care Network and NHS Business Services Authority. Paul Davies
1st October 2019 – 31st March 2020
Despite the availability of local and national guidance regarding the management of COPD exacerbations in primary care, prescribing patterns vary between practices.
Practices with high prescribing rates of rescue medication for COPD will be identified via the NHS BSA respiratory dashboard; they will then be offered individualised support using Quality Improvement methodology.
There is further useful information on our respiratory page.
Polypharmacy: supporting the pharmacist workforce event
The AHSN NENC also held an event to showcase the six projects funded through the AHSN NENC Polypharmacy Project Call and shared project outputs together with the resource toolkit developed on completion of each project. More information can be found on the Polypharmacy: supporting the pharmacist workforce event page.